The cornea is made of 5 layers, basically, the anterior part made of epithelium, Bowman’s layer and stroma, and the posterior part made of endothelium layer, and Descemet’s. In case of corneal disease, any layer, or group of layers or the whole cornea can be replaced. We are going to divide the types of corneal graft according to the layers involved.
Penetrating keratoplasty (PK) (full thickness graft): This type of graft is used in case of full or deep thickness scar that preclude the use of lamellar graft. Like in the case of severe corneal scarring due to bacterial keratitis with full thickness scar. Also, the PK could be used as an alternative for the lamellar corneal graft in case of breaching the posterior layer of the cornea during the lamellar graft surgery. 73% of PK graft survives over 5 years, although the survival rate depends on different variables. For example the survival rate for PK done because of keratoconus is 95% over 5 years, in comparison to a survival rate of 54% over the same period of time for penetrating keratoplasty due to corneal scare in relation to microbial infection.
Anterior lamellar keratoplasty: Usually the anterior lamellar keratoplasty is used to remove corneal pathology that spared the endothelium layer, in the form of Deep Anterior Lamellar Keratoplasty (DALK), in which the posterior corneal layer (Descemet’s) is lift intact with removal of the rest of the diseased cornea.
The Benefit of the DALK is that it preserves the endothelial layer, which reduces the risk of corneal graft rejection, although the visual outcome is the same as the full thickness penetrating keratoplasty. For further illustration about the DALK procedure please revert to DALK surgery under the Video section.
Femotoseond laser-assisted anterior lamellar keratoplasty (FSALK): If the corneal pathology is confined to the anterior third of the cornea, a similar thickness graft could replace the diseased layer. This procedure is termed Anterior Lamellar Keratoplasty, and is usually performed with femtosecond laser (FSALK).
The benefit of the FSALK is that it needs fewer sutures or even no sutures in comparison to both PK and DALK. Also the visual outcome is superior to both PK and DALK, as there is less interference with the corneal curvature. The rejection rate is less than the PK as less tissue is being transplanted.
Endothelial keratoplasty: The cornea maintains its clarity by an active process of continuous deterging of fluid from the corneal layers. The endothelial cells that forms the pumping machine of the cornea accomplishes this function. When the endothelial cells, which are the most posterior layer of the cornea is affected by a genetic disease like Fuch’s disease or damaged as a result of intraocular surgery like aract surgery, the cornea fail to push the excess fluid, which result in corneal clouding and eventually scarring.
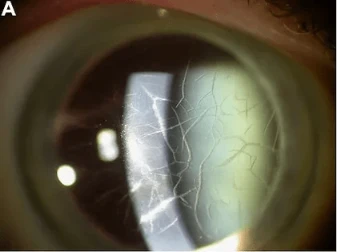
When the swollen cornea reaches the point of affecting the vision, surgery is warranted to replace the endothelium layer. Descemet’s stripping endothelial keratoplasty (DSEK) replace the diseased endothelial layer by a grafted endothelium attached to a layer of posterior stroma. It has a very good visual outcome and relatively very good visual recovery in comparison to full thickness corneal graft (PK) or DALK. Also, the rate of rejection is favourable to PK.
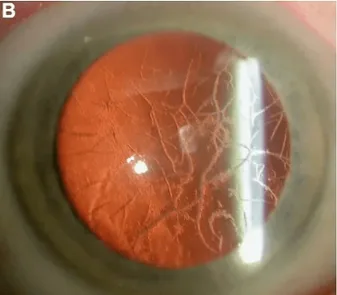
DMEK (Descemet’s membrance endothelial keratoplasty), represents the final iteration of endothelial keratoplasty, producing near-pure anatomic replacement therapy for patients with endothelial dysfunction and the visual results after DMEK seem to be better on average than the published visual results after DSEK. It involved replacing the endothelial layer along with Descemet’s to clear the cornea. The rejection rate for DMEK is very low in comparison to other corneal graft, and it is almost 0.4% over the first year after DMEK. The low rejection rate is due to the thin layer that is transplanted.
In case of high risk of failure for penetrating keratoplasty, artificial corneas could be considered, such as Boston keratoprosthesis (BKP). It is usually reserved for severe cases of corneal transplant, such as scarred cornea as a result of ocular surface inflammatory disease, resulting from chemical injury or autoimmune disease like in the case of Stevens-Johnson syndrome. Previous studies showed that the survival rate for BKP is almost 84% at 2 years and 67% at 7 years. The risk of failure varies depending on the corneal disease and it is significantly higher in ocular surface inflammatory disease. The visual acuity after BKP usually improve and almost 70% of patient will gain ambulatory vision, which helps them with daily activity.
In Summery there are a variety of corneal transplant procedures depending of the aetiology of the corneal disease and the layer that need to be replaced. The visual outcome varied depending on the surgical procedure. Survival rate of corneal graft varies significantly depending of the types of graft and the corneal disease. Corneal graft has few complications, however as rule of thumb, a partial thickness graft have reduced rate of complications and has less interference with the strength of the cornea.